Depression & Epilepsy
Any medical condition is difficult, some individuals deal with their condition better than others, but the struggle is generally still there. Many people find it hard to accept a diagnosis of epilepsy. It can be hard on themselves, family and friends. Social life takes a back seat for most
“Having epilepsy does not mean you should expect to and have to cope with depression. You have as much right to help and support as anyone else does.”
One in three individuals with Epilepsy and associated conditions will experience some form of depression/Anxiety and other mental illnesses during their lifetime. I have spoken to many people who have Epilepsy, or live with somebody who has Epilepsy and they have expressed the fact that they struggle to be motivated and sometimes to even getting out of bed in the morning after a bad day- having to face the day! Having depression can make life even more stressful than it already is.
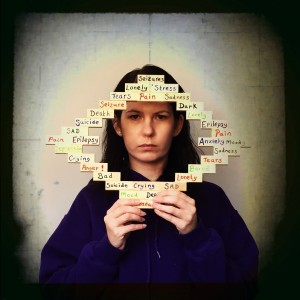
We all feel low and depressed sometimes, without it being a medical problem. Depression becomes a problem when the unhappy feelings don’t go away and it affects our daily life: eating, sleeping or being able to get out of bed. Depression isn’t just about feeling sad or ‘down’. It’s about losing interest and enjoyment in the things you used to enjoy.
If you’re depressed, you may feel worthless, hopeless, tearful, tired, restless or anxious. You may lose interest in sex or not care about your appearance. You may not be able to remember, concentrate or make decisions. You may sleep badly or wake up too early. Your appetite or weight may go up or down. You may think that life is not worth living, or think about suicide or death in general.
Depression is more likely in someone with epilepsy, studies show that depression effects 1 in 6 of those in the UK… However for people with epilepsy that number doubles to 1 in 3. This does not necessarily mean that one condition has caused the other – however having a medical condition such as Epilepsy puts more pressure upon the person for many reasons (not just the condition itself) and can therefore be a instigation. However despite having Epilepsy which can have a impact upon mood It does it mean that depression is something you just have to put up with. Women with epilepsy are more likely than men to experience depression. In fact, more women than men are diagnosed with depression in general.
People who are still having seizures are more likely to be depressed than people with controlled epilepsy. Around 22% greater that the general population.Furthermore, Epileptic patients with depression often report a poorer quality of life on global assessments and are at an increased risk of suicide as compared to the general population, 11.5 percent versus 1.2 percent, respectively.
– Anti-epileptic drugs (AEDs) and depression
Depression can sometimes be a side-effect of AEDs. This is particularly the case for older drugs such as phenobarbital, phenytoin and primidone. These side-effects are dose-related. This means that the higher the dose you are taking, the more likely you are to become depressed. If you take more than one kind of AED, this can also increase your chance of becoming depressed.
(I take 7 different types)
If you are affected by depression, don’t suffer in silence. Speak with your family doctor, epilepsy nurse or epilepsy specialist. Tell them as much as you can about when you started feeling depressed, and how it is affecting you.
Side effects from medication can also increase the risk of depression. Anti-seizure drugs may affect the mood centers in the brain. Many different medications are used to treat epilepsy. Barbiturates, including Phenobarbital, may contribute to depression more than other anticonvulsant medications. Benzodiazepines, levetiracetam, topiramate, and vigabatrin may also dampen your mood. Your doctor may switch you to another drug if your medication is the cause of your depression.
Treating depression and epilepsy at the same time can be tricky. Medications can interact with each other and lead to a worsening of symptoms in one or both conditions. It’s common to try a variety of medications to determine which combination is the best fit. Some Doctors will not treat the depression at all.
I went to my GP, I was in severe depression, I was going through a really bad spell with my Epilepsy. I was crying all the time. Didn’t want to do anything or get out of bed. At this point I’m ashamed to say it but I wanted to die. My GP sent me home with nothing except a “im sorry your feeling like this” !! Despite that I was in that state – crying in front of them. (It does shamefully depend upon the GP you see…. the key is to make an appointment to see another GP before you leave the building and make the receptionists aware why). I had my mum and so I had support – I made another appointment with a different dr for another time. If you have no one with you at the time though my advice is to not leave without letting the receptionists know your predicament and how you feel.
Eventually when offered help the treatment you are offered for your depression will depend on not only your GP but also how seriously it is affecting you. You might be offered antidepressants or talking treatments, such as counselling or cognitive behavioural therapy. Some people will need a combination of treatments. If you are very unwell, and drugs don’t help, or you are considered to be at risk of suicide, you could be admitted to hospital.
When your doctor is making a decision about your treatment, they will have to carefully consider the benefits and risks. This is because some antidepressant drugs can make seizures more likely. This is particularly the case if they are given in high doses.
Some AEDs such as sodium valproate, carbamazepine, lamotrigine and oxcarbazepine can help to stabilise people’s moods. This can lessen the risk of depression coming back in the future.
There are herbal and complimentary options however It’s really important to speak with your doctor or epilepsy nurse, before you try any complementary or alternative treatments. This is because these treatments may interfere with your anti-epileptic drugs. An example of this is St John’s Wort, which can cause seizure which would make your condition worse.
It’s important to remember that depression and epilepsy are both manageable medical conditions. You may be at a higher risk for depression if you have epilepsy. But there are steps you can take to overcome your challenges and live a happy, productive life.
I eventually ended up with one of the most kind Drs regarding depression in medical conditions in the practice where I go. I have my ups and downs but on the whole I do ok with my friends and family around me. In fact this blog is going to be a surprise for a few I think (I’m pretty good at hiding my feelings).
Remember to be strong, and just because you are feeling low now – you can overcome these stages with help. Don’t be afraid to ask for it. Reach out to your friends and family. It has taken me a couple of years to get the courage to post this blog and even mention Ive struggled. It’s nothing to be ashamed of. It’s stigma again and that is all. People think I’m strong – On the whole I feel like I can be, however there are these times when everyone needs help.
“Just because you’re struggling now, you will overcome it in the end”
HELPFUL EMERGENCY CONTACTS
If you are in need of someone to talk to here are some useful contacts. Don’t be afraid to call them.
The Samaritans: Whatever you’re going through, call us free any time, from any phone on 116 123. Email: jo@samaritans.org Website: www.samaritans.org
Campaign Against Living Miserably (CALM): for men Call 0800 58 58 58 5pm to midnight every day Website: www.thecalmzone.net
Papyrus – for people under 35 Call 0800 068 41 41 – Monday to Friday 10am to 10pm, weekends 2pm to 10pm, bank holidays 2pm to 5pm Text 07786 209697 Email pat@papyrus-uk.org
The Silver Line – for older people Call 0800 4 70 80 90
MIND: 0300 123 3393 info@mind.org.uk
Text: 86463


Recent Comments